Summary of Kidney Cancer Highlights from ASCO GU 2023
Source: International Kidney Cancer Coalition (IKCC)
This year’s American Society of Clinical Oncology Genitourinary Cancers (ASCO GU) Symposium was held from 16-18 February 2023, in San Francisco, CA, USA. The presentations are available to view on the ASCO website. Some affiliates of the International Kidney Cancer Coalition (IKCC) went to the meeting to keep up to date with the care and treatment of patients with kidney cancer. A brief Take home messages section is followed by more in-depth review of selected abstracts.
Please note: The following summary was prepared for the benefit of patient advocates and patient organisations around the world who focus on kidney cancer. While this summary has been medically reviewed, the information contained herein is based upon public data shared at this meeting and is not intended to be exhaustive or act as medical advice. Patients should speak to their doctor about their own care and treatment.
Take home messages
- In Abstract 653, the IKCC presented the first results from the 2022 Global Patient Survey. The survey showed that there was a lack of genetic testing and understanding about kidney cancer, clinical trials, and the psychosocial effect of the disease. Importance: The survey suggested that better communication between patients and doctors is needed. This will help patients learn about genetic testing, how to access treatments by taking part in clinical trials, and where to get counselling if needed.
- In Abstract 663, KCCure presented early results from their patient survey on treatment given to patients to stop their cancer from coming back after surgery (adjuvant treatment) mostly involving patients from the USA. Importance: Patients need to know about the risks and benefits of adjuvant treatment through good communication with their doctors. Patients must have all the information they need to be involved in the decision to take adjuvant treatment.
- In Abstract 679, results from the clinical trial where pembrolizumab was given to patients to stop their cancer coming back after surgery (adjuvant treatment) were assessed according to the risk of the cancer returning. Importance: This study showed that patients who had had metastases removed and were cancer-free had decreased rates of the cancer coming back when taking pembrolizumab compared with patients who were taking placebo.
- In Abstract 600, a study looking at patients with brain metastases from kidney cancer showed that patients treated with immunotherapy combinations have better survival than those treated with a VEGFR TKI. Treatments such as brain surgery or stereotactic radiotherapy (radiation beams targeted directly at the metastases) also improved survival in these patients. Importance: For patients diagnosed with brain metastases from kidney cancer, immunotherapy combinations, surgery, or stereotactic radiotherapy can help them live longer.
- In Abstract 603, combination therapies continue to improve patient survival. New information from a trial with nivolumab plus cabozantinib shows that after more than 3 years follow-up, patients continue to benefit from the treatment. However, the study confirmed that there is no test that can predict which patients will benefit from this treatment (abstract 608). Importance: For patients, the nivolumab plus cabozantinib combination has long lasting effects on survival. But there are no tests to predict for which patients this combination works best.
- In Abstract 605, the results from a study using a combination of three medicines; cabozantinib, ipilimumab and nivolumab showed that the triple combination helped patients with intermediate-risk kidney cancer more than those with poor-risk kidney cancer. Importance: Although this study shows that cabozantinib, ipilimumab and nivolumab works better in patients with intermediate-risk disease, the study is still ongoing, and the results might change.
- In Abstract 606, early results show that cabozantinib is effective as a second treatment for advanced kidney cancer after the first treatment with immunotherapy has stopped working. This study provides more choice for patients as a second treatment when their first treatment no longer works. It also seems that the time of day when immunotherapy is given may affect survival (abstract 678). When given earlier in the day patients respond better and survival is improved. Importance: Cabozantinib provides more choice for patients as a second treatment when their first treatment no longer works. Patients should be treated with immunotherapy earlier in their treatment plan, if possible.
- In Abstract 660, a study using a mindfulness programme on a smartphone has shown that the programme could improve health-related quality of life and decrease anxiety, fear of the cancer returning, and fatigue. Importance: If patients have access to a smartphone, this app could help improve the quality of life of patients with kidney cancer.
- Finally, in LBA602, a small study looked at using a weakly radioactive protein (an antibody called 89Zr-DFO-girentuximab) to identify kidney cancer on scans. This study confirms that 89Zr-DFO-girentuximab is well tolerated and can accurately identify kidney cancer on a PET/CT scan. Importance: This product could help to diagnose kidney cancer more accurately without the need for a biopsy.
Summaries
Abstract 653: How do patients around the world experience the diagnosis, burden, and management of kidney cancer?
The number of patients suffering kidney cancer continues to rise around the world, increasing the burden on patients, their families and healthcare systems. Little is known about how kidney cancer treatment and patient experiences vary between countries. This was a poster presentation of the third biennial worldwide International Kidney Cancer Coalition (IKCC) Global Patient Survey of the diagnosis, management, and burden of kidney cancer.
The aim of the survey was to improve understanding and contribute to reducing the burden of kidney cancer. Patients and caregivers completed a 35-question survey to identify differences between countries in the diagnosis, burden, and management of kidney cancer. The survey was distributed in 15 languages via IKCC’s 49 Affiliate Organisations and social media. The survey was designed to look at patient education, experience and awareness, access to care and clinical trials, best practices, quality of life, and unmet psychosocial needs.
Over 2,200 people from 39 countries responded to the survey, 1,655 of which were patients. The data were independently analysed. The poster is available on the IKCC website. In terms of diagnosis, nearly half (47%) had advanced disease and 11% had localised disease. The remaining people had no evidence of disease. Most patients (58%) had clear cell kidney cancer, and there was a high proportion of patients with non-clear cell disease (31%).
Nearly half of the patients with the greatest risk of hereditary kidney cancer are not receiving appropriate counselling.
In terms of clinical trials, just over a third of patients had been asked to take part in a clinical trial and 70% of these agreed. Nearly two thirds of these patients were satisfied with their experience in a clinical trial.
With respect to wellbeing, 20% of patients felt their emotional wellbeing since diagnosis was affected by anxiety about their kidney cancer. 28% reported that fear of their cancer coming back affected their emotional wellbeing. 11% said their emotional wellbeing was affected by sadness or depression.
The survey identified that there was a lack of genetic testing among people at risk of kidney cancer. The survey also showed that there was a lack of understanding about the disease, genetic testing, clinical trials, and the psychosocial affect. The survey also provided patient’s ideas about biopsies, physical activity, and follow-up schedules. Real world evidence provides opportunities to improve communication about diagnosis, psychosocial affect, and clinical trials.
The IKCC and its global Affiliate Organisations will be using these results to ensure that the patient’s voices are heard. The survey will also be used to suggest future projects. Individual countries can use their reports to advance their understanding of patient experiences and to support improvements in local care.
Adjuvant therapy for kidney cancer
Abstract 663: Patient perception of benefits and risks of adjuvant therapy for kidney cancer
KCCure presented some early data from their survey of over 1000 patients from 28 countries, mostly the USA (85%). 36% had stage 3 disease and 18% were offered treatment to stop their cancer from coming back after surgery (adjuvant therapy). Two thirds accepted adjuvant therapy, 19% declined, and 14% were enrolled in a clinical trial.
Nearly half of the people in the survey thought that their risk of the cancer coming back was higher (by about 10-15%) than what their doctor thought. About a quarter of patients overestimated the benefit of adjuvant therapy, thinking it would reduce their risk of the cancer coming back by 50% or more. For most people, they agreed that a decision needed to be made and wanted to be involved in the decision. Most doctors explained what adjuvant therapy was and there were high levels of shared decision-making (80-90%). For people with a high-risk of their cancer coming back, they were prepared to tolerate the side effects and reduced quality of life to prevent this.
This survey highlights the importance of effective communication between patients and their doctors on the risks and benefits of adjuvant therapy. It also highlights the importance of informed shared decision-making.
Abstract 679: Adjuvant pembrolizumab for different risks and stages of kidney cancer
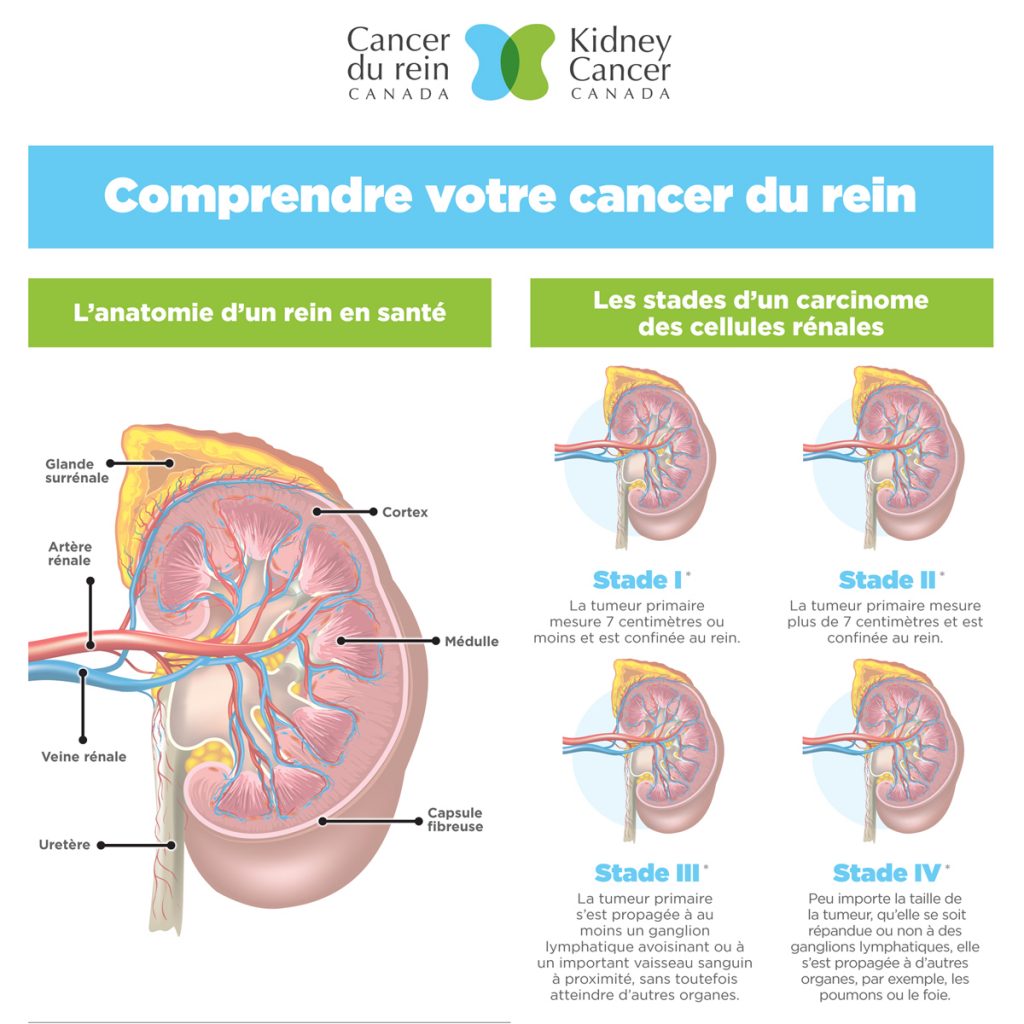
Surgery to remove the kidney, either partly or entirely (partial or radical nephrectomy), is the standard of care for large, high-risk kidney cancers that have not spread outside the kidney. The cancer can come back (recurrence) after nephrectomy in some patients. Adjuvant therapy is additional treatment that is taken after surgery to reduce the risk of the cancer from coming back.
Currently, there isn’t a standard adjuvant therapy for high-risk kidney cancer that has not spread outside the kidney. Trials with vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitors (TKIs) that block the blood supply to the cancer have shown little benefit for patients.
However, immunotherapy (medicines that stimulate the immune system to attack cancer cells) is now being tested in clinical trials as potential adjuvant therapies to see if they can stop the cancer from coming back in other parts of the body.
In the KEYNOTE-564 clinical trial the immunotherapy medicine called pembrolizumab (given by an infusion into a vein) has been shown to improve cancer-free survival after nephrectomy for kidney cancer patients at high-risk of their cancer returning. The results from KEYNOTE-564 have been looked at to see how different groups of patients responded to pembrolizumab. The groups were based on the risk of the disease returning and the stage of the cancer when the patient entered the study.
The results from this clinical trial were reported last year. The results showed that after 2.5 years, adjuvant pembrolizumab reduced the risk of the cancer returning by about one third. Also, the number of patients experiencing serious or life-threatening side effects with pembrolizumab was less than 10%.
994 patients were enrolled in the trial, of which nearly three quarters had intermediate-risk disease and 20% had high-risk disease. The remaining patients (6%) had metastases that had been removed and they were cancer-free. Patients were followed-up for 30 months.
The results were consistent with those already reported. Of all the groups looked at, the patients who had had metastases removed leaving them without any evidence of disease had the biggest difference in rate of cancer- free survival compared with placebo (78.4% versus 37.9% after 2 years).
The results from the different groups of patients according to risk and stage of disease are consistent with previous results from this trial: Adjuvant pembrolizumab improves cancer-free survival in all patients with high-risk kidney cancer compared with placebo. These results further support the use of adjuvant pembrolizumab as a standard treatment for patients with kidney cancer at high-risk of recurrence.
However, patients should consider their situation carefully with their doctor and discuss the potential risks and benefits of adjuvant pembrolizumab. Without a test to predict which patients might benefit from treatment or who might suffer serious side effects, some patients may be given treatment that they don’t need, and they may suffer from the potentially serious side effects of pembrolizumab unnecessarily. This needs careful consideration.
Abstract 600: Outcomes of patients with brain metastases from kidney cancer treated with first-line therapies
When kidney cancer spreads to other parts of the body, this is called metastatic or advanced kidney cancer. The cancer can spread to organs such as the lymph nodes, lungs, liver, bones, and brain. Medicines that block the cancer blood supply (VEGFR TKI tablets) or immunotherapy medicines that stimulate the immune system to attack the cancer are often used to help patients with metastatic kidney cancer live better and longer. However, because people with spread of their kidney cancer to the brain are often excluded from clinical trials, there is not a lot of information about the outcomes of these patients when treated with first-line therapies.
In this study, 775 patients with brain metastases from kidney cancer were assessed. About 10% of them were taking immunotherapy combination treatments (either immunotherapy plus VEGFR TKI, or immunotherapy plus immunotherapy), while the remainder were on a VEGFR TKI (sunitinib or pazopanib). A quarter of the patients on an immunotherapy combination also had whole brain radiotherapy, while more than half of the patients on a VEGFR TKI were given this treatment.
The patients who were treated with an immunotherapy combination had the best overall response to treatment in all disease sites. 3.4% had a complete response, just over a quarter had a partial response and nearly 40% had stable disease. However, in the patients treated with a VEGFR TKI, less than 1% had a complete response, nearly 30% had a partial response, and just over a third had stable disease.
For patients with favourable- or intermediate-risk disease, treatment with an immunotherapy combination, brain surgery to remove metastases, and stereotactic radiotherapy (radiation beams targeted directly at the metastases) improved overall survival time for patients with brain metastases from kidney cancer.
Patients with brain metastases have longer survival times when treated with immunotherapy combinations than single VEGFR TKI treatment. Treatments directed at the metastases, such as brain surgery or stereotactic radiotherapy also improved survival time in these patients.
Combination treatments continue to show promise as first treatments
Advanced kidney cancer is often treated with a combination of medicines; either two infusions of immunotherapy (nivolumab and ipilimumab) or immunotherapy (avelumab, pembrolizumab or nivolumab) plus a VEGFR TKI tablet (axitinib, lenvatinib, or cabozantinib). Many similar combinations have been tested and others are in development.
Combination therapies continue to be of great interest at ASCO GU 2023, with the presentation of updated results from some ongoing studies. But crucially, none of these studies can help us with the critical question; which combination of treatments is best for an individual patient with advanced kidney cancer?
Abstract 603: Three-year follow-up with cabozantinib plus nivolumab: does the benefit continue?
The phase 3 clinical trial, CheckMate-9ER, shows that cabozantinib (a VEGFR TKI tablet) used together with nivolumab (an immunotherapy infusion) is better than VEGFR TKI alone at shrinking the cancer, and for survival in patients with advanced kidney cancer who had not previously taken any treatment.
After more than three years, the combination of cabozantinib plus nivolumab continues to improve survival, control the cancer, and shrink the cancer on scans compared with sunitinib (a VEGFR TKI tablet).
The time to when the treatment stopped working and the cancer started growing again was doubled with the combination treatment compared with sunitinib (16.6 months versus 8.4 months, respectively). Average overall survival time was just over 4 years with the cabozantinib plus nivolumab combination, compared with nearly 3 years for sunitinib. Additionally, the number of patients who responded to treatment doubled with the combination (56%) compared with sunitinib (28%) and 12% of the patients had a complete response compared with 5% for sunitinib. Also, the average duration of the response was longer for the patients on the combination (23.1 months), than for those on sunitinib (15.2 months).
Slightly more patients experience side-effects with the combination (97% versus 93%), and the side effects were more severe. This was similar to previous studies of this combination. However, only 7% of patients stopped combination treatment because of side effects.
After more than 3 years follow-up, patients continue to benefit from the cabozantinib plus nivolumab combination. Average overall survival time has improved by nearly a year since last year, and patients continue to respond to treatment, regardless of the severity of their disease.
Abstract 608: Biomarkers to predict patient response to a combination of nivolumab plus cabozantinib
Currently, it is not known why some people respond to combination treatments, when others don’t. In this study, patients from the CheckMate-9ER study were used to look for natural substances or genes (also called biomarkers) in people with advanced kidney cancer that can be used to predict their response to the combination of nivolumab plus cabozantinib. The researchers looked at biomarkers called CD8 T cells and PD-L1, as well as the genes of people with advanced kidney cancer taking the combination treatment.
After more than 3.5 years of follow-up, survival was improved for the patients taking the nivolumab plus cabozantinib combination. The time to when the drug stopped working and the cancer started growing again (progression-free survival) and overall survival time were better with the combination treatment than with sunitinib, regardless of whether the patient had the PD-L1 biomarker in their blood. However, PD-L1 levels of less than 1% were linked with longer average progression-free survival in the patients taking sunitinib only. A higher level of CD8 T cells was linked with improved progression-free survival in the patients who were treated with the combination, but not sunitinib. All the genetic tests did not predict patient outcomes in this study.
In this test for biomarkers, none were able to predict the effectiveness of nivolumab plus cabozantinib in patients with advanced kidney cancer.
Abstract 605: The effectiveness of a triple combination of cabozantinib, nivolumab and ipilimumab for previously untreated patients with different risks for kidney cancer
Cabozantinib may improve the effectiveness of immunotherapy. COSMIC-313 is the first study to combine cabozantinib with two immunotherapy medicines, nivolumab and ipilimumab. This combination of three medicines is compared with a combination of ipilimumab, nivolumab and placebo for the treatment of people with intermediate- or high-risk advanced kidney cancer.
855 patients were assessed in this phase 3 study. Patients were randomly assigned to receive either nivolumab and ipilimumab plus cabozantinib or nivolumab and ipilimumab plus placebo. The study is double-blind, meaning both the doctor and the patient do not know which treatment they are on. All patients had clear cell kidney cancer that was of intermediate- or high-risk.
Preliminary results from the clinical trial showed that adding cabozantinib to nivolumab plus ipilimumab significantly increased the time to when the treatment stopped working and the cancer started growing again (progression-free survival). Average progression-free survival was not reached for the triple combination, but for the ipilimumab plus nivolumab combination it was just over 11 months. Patients were assessed according to the severity (risk) of their cancer.
Overall, three quarters of the patients in the study had intermediate-risk cancer, and one quarter had poor-risk cancer. In the patients with intermediate-risk cancer, progression-free survival was improved with the triple combination, and response to treatment and control of the disease was higher compared with ipilimumab plus nivolumab (45% versus 35% and 88% versus 75%, respectively). For the patients with poor-risk disease, there was no difference in progression-free survival, but control of the disease was higher with the triple combination (81% versus 64%).
Serious and life-threatening side effects were reported by 74% of patients on the triple combination, and 42% on ipilimumab plus nivolumab in patients with intermediate-risk disease. In patients with poor-risk disease, serious and life-threatening side effects were reported in 67% of patients with poor-risk disease versus 38% for intermediate-risk disease. Side effects led to the treatment being stopped in 14% of patients on the triple combination versus 5% on the double combination for intermediate-risk patients and 5% versus 4% for poor-risk patients, respectively.
This subgroup analysis of the COSMIC-313 data suggests that the benefit of cabozantinib plus ipilimumab plus nivolumab is primarily for patients with intermediate-risk kidney cancer. However, the trial is continuing for the collection of overall survival data.
Abstract 606: Cabozantinib as a second-line treatment after immunotherapy in patients with advanced kidney cancer
The standard of care for the first-line treatment of advanced kidney cancer is usually immunotherapy. There is a lack of information about the use of cabozantinib after the use of first-line immunotherapy. The CaboPoint study looks at using cabozantinib as a second-line treatment after immunotherapy has stopped working.
CaboPoint is an ongoing phase 2 study of cabozantinib in people with locally advanced or metastatic kidney cancer that cannot be removed with surgery. These people have been treated with immunotherapy, but their cancer has started to grow again. There are two groups in the study: group A was treated with ipilimumab plus nivolumab, and group B was treated with an immunotherapy plus a VEGFR TKI. When their first treatment stopped working, both groups of patients were treated with cabozantinib until the end of the study (at least 18 months). Here, results from the first 3 months of treatment with cabozantinib are reported.
At the time, 88 patients had 3 months of cabozantinib treatment. At this early stage in the study, cabozantinib has shown some effectiveness in patients with advanced kidney cancer after their first treatment with immunotherapy combinations had stopped working, regardless of which first treatment they had. The CaboPoint trial is ongoing, and the final analysis is expected in September 2023.
Abstract 678: How the time of day of immunotherapy infusion affects disease outcomes in patients with metastatic kidney cancer
Recent studies have suggested that the time of day when an immunotherapy infusion is given might affect the survival of patients with cancer. In this study, the researchers wanted to see if this was the case for patients with metastatic kidney cancer.
Patients with metastatic kidney cancer were treated with nivolumab, either alone or in combination with ipilimumab as a first or second treatment. Patients were assessed in two groups: those who had more than three quarters of their infusions before 4.30 pm (the ‘early’ group), and those who received a quarter or more of their infusions after 4.30 pm (the ‘late’ group). A total of 145 patients with metastatic kidney cancer were included in the study. About three quarters of the patients had intermediate- or poor-risk disease. Most patients (75.9%) were in the early group.
Average overall survival time for all patients in the study was 41.7 months. The response rate to treatment was greater in the early group than the late group (32.7% versus 25%, respectively). The average overall survival time was 46.3 months for the early treatment group compared with 41.7 months for the late treatment group.
These results show there is an increase in response to treatment and overall survival time when immunotherapy is taken earlier in the day. Larger, randomised, and controlled clinical trials are needed to confirm these results.
Abstract 660: Improved health-related quality of life with the use of an online mindfulness tool in patients with metastatic kidney cancer on immunotherapy
Randomised clinical trials have previously shown the benefit of mindfulness in multiple cancer types, but there is limited information for metastatic kidney cancer. This study looked at the effect of an online mindfulness tool on the health-related quality of life of people with metastatic kidney cancer taking immunotherapy.
Metastatic kidney cancer patients who were being treated with immunotherapy and had symptoms of anxiety, fear of cancer progression, and fatigue were included in the study. The patients needed to have access to a smartphone and the internet and had not taken part in a mindfulness programme for at least 5 years. The study looked at the Mindfulness-based Cancer Survivorship Journey using the Am smartphone app (AmDTx). Patients used the app for 20-30 minutes each day for a minimum of 4 days a week for 4 weeks. Patients were assessed at the start of the study (baseline), and at weeks 2, 4 and 12 using various health-related quality of life scoring systems.
41 patients were recruited across 7 sites in Brazil and the USA. Most patients were on ipilimumab plus nivolumab, nivolumab alone, or pembrolizumab plus axitinib. Symptoms of anxiety and fear of cancer returning significantly decreased during the study. Health-related quality of life also increased. There were no differences based on disease characteristics or type of treatment.
This study suggests that smartphone-based mindfulness programmes could improve health-related quality of life and decrease anxiety, fear of the cancer returning and fatigue. This low-cost and easily accessible programme may provide an important alternative to face-to-face psychosocial support for patients with metastatic kidney cancer. This programme should be assessed in larger randomised clinical trials for metastatic kidney cancer patients.
Abstract LBA602: Results from a phase 3 study of 89Zr-DFO-girentuximab for PET/CT imaging of kidney cancer
Researchers are looking for better ways to diagnose kidney cancer. Currently, diagnosis is made using scans, which cannot tell the difference between benign and cancerous tumours, and biopsy, which involves surgery and is not always accurate. There is, therefore, an unmet need for an accurate test to diagnose kidney cancer to guide patient management.
Girentuximab is an antibody that attaches to an enzyme called carbonic anhydrase IX (CAIX). This enzyme is found in clear cell kidney cancer tumours. 89Zr-DFO-girentuximab (TLX250-CDx) is a product made from combining a weakly radioactive molecule called zirconium Zr 89 with girentuximab. When given to humans, 89Zr-DFO-girentuximab binds to carbonic anhydrase IX in kidney cancer tumours and can help to tell the difference between kidney cancer, normal tissue, and other tumours.
Patients who were scheduled to have a partial nephrectomy within 90 days were given 89Zr-DFO-girentuximab 10 days before surgery and then had a PET/CT scan 5 days later. The scans were assessed independently to determine whether the patient had kidney cancer. Both the sensitivity and accuracy of the scans where assessed.
There were 300 patients in the study, two thirds of whom had clear cell kidney cancer. The results were assessed independently by 3 radiographers. The average sensitivity was 86%, and the average accuracy was 87%. Positive predictive values for kidney cancer were more than 90%. There were only two treatment-related side effects.
This study confirms that 89Zr-DFO-girentuximab is well tolerated and can accurately identify kidney cancer from a PET/CT scan. This is promising for the management of kidney cancer patients.
Acknowledgements:
Editor:
Dr Cristiane Bergerot (BR)
Medical Reviewers:
Professor Axel Bex (NL/UK)
Dr Rachel Giles (NL)
Dr Eric Jonasch (USA)
Medical Writer:
Dr Sharon Deveson Kell (UK)