This discussion guide is intended for those living with advanced (metastatic) kidney cancer and can be used to support conversations with your doctor and/or medical team when making decisions about systemic therapy to treat your cancer. Systemic therapy refers to any type of cancer treatment that targets the entire body.
View or download the discussion guide
Bring the guide to appointments with your medical oncologist, including your first one or any follow-up appointments with your medical team. Many of these topics will be covered by your doctor, but if not, this guide can help you understand more about the options available to you and arm you with the questions you need to make an informed, joint decision with your doctor and/or medical team.
ABOUT SYSTEMIC THERAPY
For advanced kidney cancer, systemic therapy options include targeted therapy, immunotherapy, or a combination of these. Some systemic therapies can be taken in tablet form at home, while others are given intravenously (entering through a vein) at a cancer centre or infusion clinic.
The below questions can be helpful as you learn more about your medical team and your treatment options.
What is the role of my medical oncologist and/or radiation oncologist?
Who else makes up my medical team? Who is my main point of contact for questions/concerns?
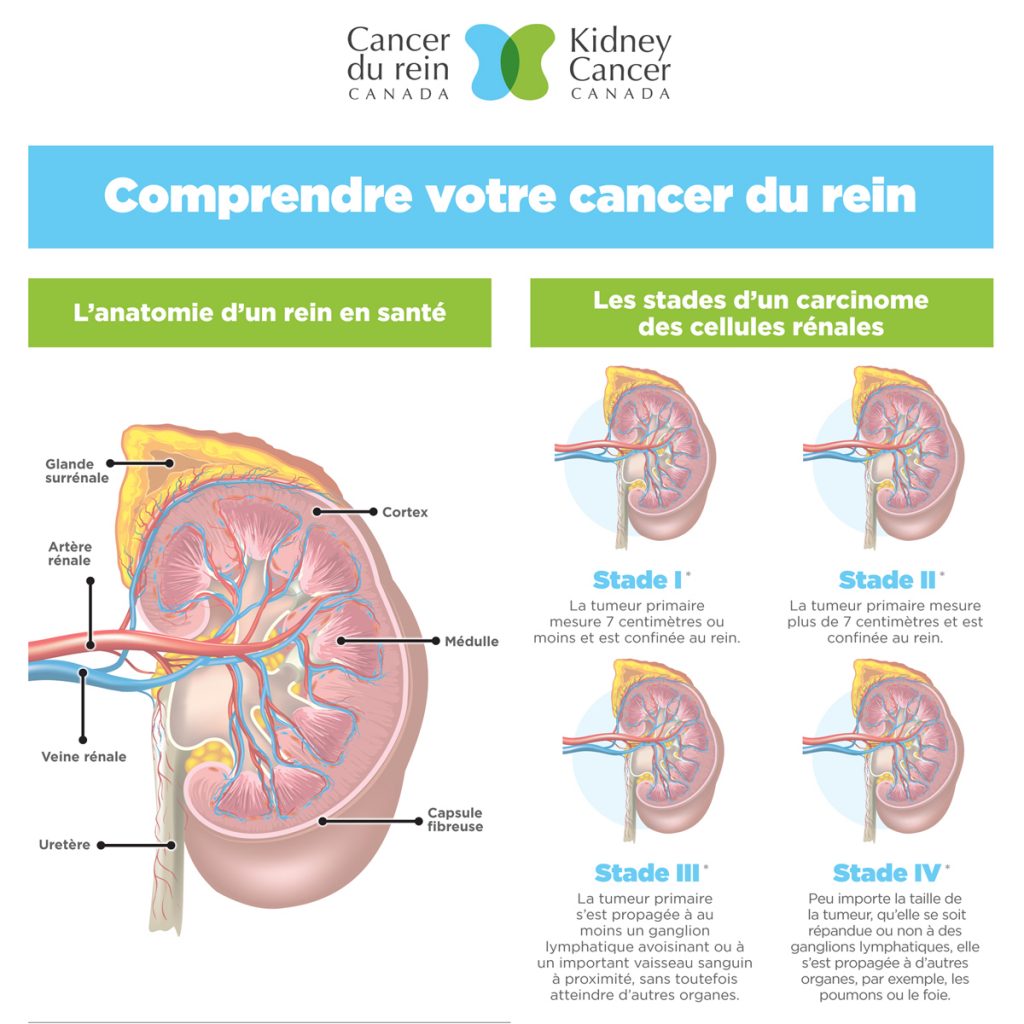
What does the type/subtype, and stage of my kidney cancer mean for my treatment plan?
Why is systemic therapy recommended for me? How is it different than chemotherapy?
What are the differences between targeted therapies and immunotherapies?
UNDERSTANDING TREATMENT OPTIONS
Whether you’re starting or continuing a systemic therapy, there are important questions to ask that can determine your treatment path depending on where you live in Canada, your health insurance coverage, and the current recommended guidelines for approved treatments.
The below questions can prompt discussion about the treatment path your doctor is recommending and why it’s the best option for you at this point in your care.
What treatments are available/covered by my provincial health insurance and how do I get access? Will I have to pay for the drug?
What treatment is the best option for me, and why? Will it give me a better quality of life, more time, shrink my tumour, etc.?
Does the treatment you are recommending now make me ineligible to receive other treatments in the future?
What does first line, second line, third line treatment mean?
What happens if my current treatment fails? What are my other options?
ABOUT YOUR TREATMENT
It’s important to communicate with your medical team and tell them everything you are experiencing. There are things they can do to adjust dosing/dosing schedules or manage potential side effects.
The questions below will prompt discussion, to ensure you have the best experience possible.
How can I prepare for treatment? Are there lifestyle changes you recommend?
What are the potential side effects of this treatment, and how can they be managed?
What should I look out for in terms of side effects? When should I contact my doctor?
Can my dose be adjusted and/or reduced if I experience side effects?
Can I take breaks or adjust the dosing schedule of my treatment if I have travel plans, an important event, or other commitments?
If my dose is adjusted, does it impact the effectiveness of my treatment?
MONITORING & FOLLOW-UP
Monitoring how your cancer responds to treatment is an important part of managing the disease. It’s also an opportunity for your medical team to check in on how you are doing. Your medical oncologist will typically send you for imaging every 8-12 weeks, which may include CT scans, MRIs and/or bone scans. Appointments and bloodwork with your medical team will happen more frequently.
The questions below will help you navigate conversations about monitoring and progression while under the care of your medical oncologist / medical team.
What does monitoring entail? Why is it important?
How and when will we know if my treatment is working?
What follow-up tests and imaging will I need? How often do I need them?
How is ‘progression’ defined at this stage (is there spread, growth of existing tumours, etc.)?
What happens next if my cancer grows or progresses?
The guide was developed with the support of Ipsen Biopharmaceuticals Canada Inc.