Sometimes people think they are at risk for developing cancer if they have 1 or 2 family members with cancer. Having a family member with cancer doesn’t mean that your family has an inherited or hereditary cancer syndrome. Only a small number of cancers are considered to be hereditary.
However, people with a family history of kidney cancer in a close relative (such as a parent, brother, sister, or child) do have a higher risk of developing kidney cancer.
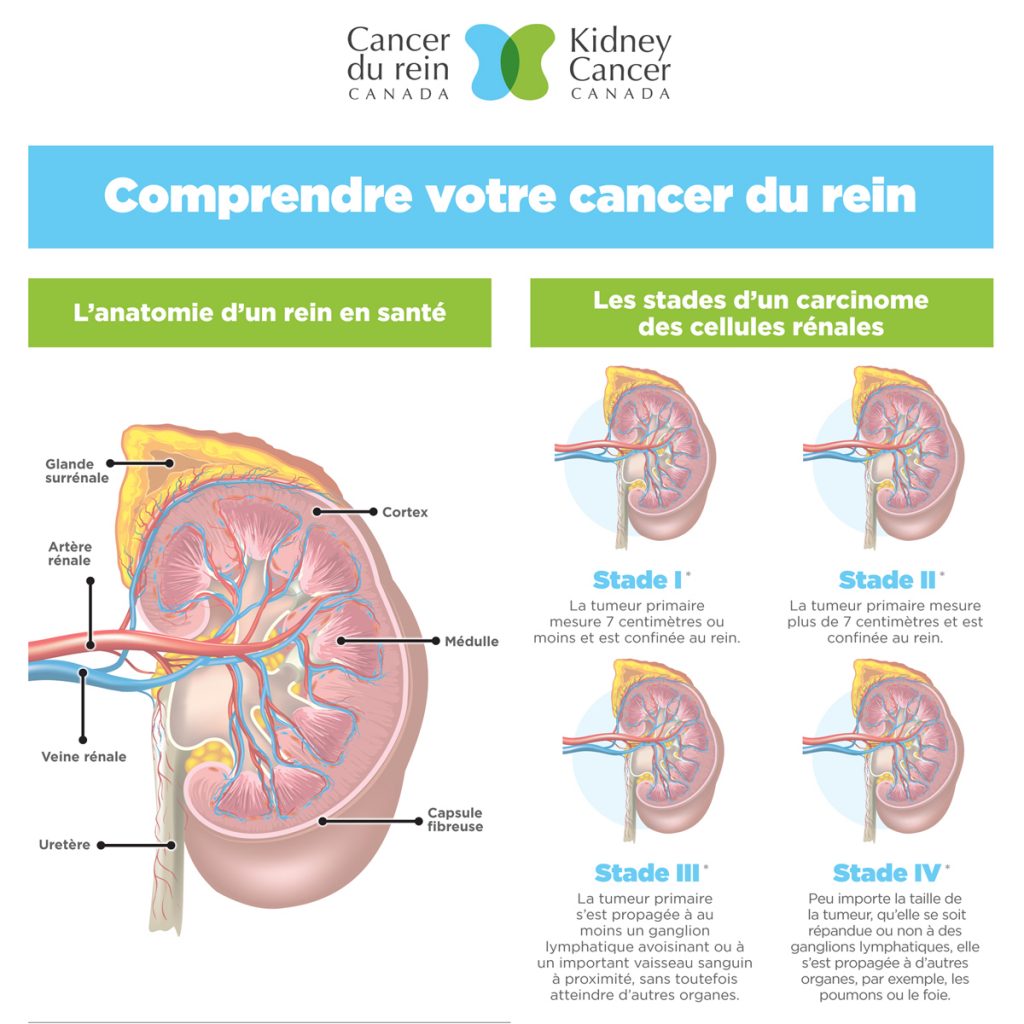
The risk of developing kidney cancer is increased if the family member was diagnosed:
- At a younger age than usual, such as before the age of 45
- With cancer in both kidneys
- With more than one tumour in the same kidney
The factors listed above give a clue that the kidney cancer could be due to an inherited gene mutation that predisposes family members to a hereditary kidney cancer syndrome.
HEREDITARY KIDNEY CANCER
Genes are present in pairs, meaning that we have two copies of every gene. One copy of every gene is inherited from our mother and the other copy from our father. Most hereditary disorders that predispose a person to kidney cancer are inherited in a dominant fashion. This means that one copy of the gene has a mutation, while the other copy doesn’t. If one parent has a hereditary condition, they have a 50% chance of passing a mutated gene onto each child. Each child also has a 50% chance of not inheriting the mutated gene.
IMPLICATIONS FOR FAMILY MEMBERS
Knowing that a family member carries a gene mutation that predisposes them or makes them more susceptible to developing cancer, can also help identify other family members who carry the same mutation and who are therefore also at risk of developing cancer. Testing family members who do not have cancer is called predictive genetic testing and this is done to find out if the family members carry the same mutation that their relative is known to have. Family members who are found to carry a mutation often have personalized checkups and testing based on the specific gene mutation. These measures are done to help detect cancer early, so that it can be treated and give the person the best possible benefit from early treatment.
TREATING HEREDITARY KIDNEY CANCER
Each hereditary kidney cancer syndrome is often associated with a particular type of kidney cancer caused by mutations in different genes, with unique cancer cell features and differences in how they respond to treatment. Understanding the genetics behind kidney cancer has served as a framework for developing treatments that are better able to target kidney cancers caused by related groups of genes. For example, drugs like sunitinib (Sutent®), sorafenib (Nexavar®), everolimus (Afinitor®), temsirolimus (Torisel®), pazopanib (Votrient®) and axitinib (Inlyta®) are known to target genes that cause kidney cancer related to the von Hippel-Lindau (VHL) and associated genes. Everolimus, which also targets genes associated with tuberous sclerosis complex (TSC) and its related genes, may be used in people with TSC who develop kidney tumours called renal angiomyolipomas. Other new therapies that target specific groups of genes are being developed and studied.
SECTION REFERENCES:
Canadian Cancer Society. Risk Factors for Kidney Cancer. 2016
Canadian Cancer Society. Inherited Cancer Risk. 2016.
Haas NB, Nathanson KL. Hereditary renal cancer syndromes. Advances in Chronic Kidney Disease. 2014; Jan; 21(1):81-90.
Ho TH, Jonasch E. Genetic Kidney Cancer Syndromes. Journal of the National Comprehensive Cancer Network. 2014; September;12(9):1347-1355.
Linehan WM. Genetic basis of kidney cancer: role of genomics for the development of disease-based therapeutics. Genome Research. 2012; Nov;22(11):2089-100.
Linehan WM, Pinto PA, Bratslavsky G, et al. Hereditary kidney cancer: unique opportunity for disease-based therapy. Cancer. 2009; May 15;115(10 Suppl):2252-61.
U.S. National Library of Medicine. Genetics Home Reference: Your Guide to Understanding Genetic Conditions. Help Me Understand Genetics. Published: 12/1/2016.
Updated 2017-02-01