Summary of Kidney Cancer Highlights | ESMO 2023
Source: International Kidney Cancer Coalition (IKCC)
This year’s European Society for Medical Oncology (ESMO) Congress was held from 20-24 October 2023, in Madrid, Spain. The presentations are available to read on the ESMO website. Some affiliates of the International Kidney Cancer Coalition (IKCC) went to the meeting to keep up to date with the care and treatment of patients with kidney cancer. In this report, a brief “Take home messages” section is followed by more in-depth review of selected abstracts.
Please note: The following summary was prepared for the benefit of patient advocates and patient organisations around the world who focus on kidney cancer. While this summary has been medically reviewed, the information contained herein is based upon public data shared at this meeting and is not intended to be exhaustive or act as medical advice. Patients should speak to their doctor about their own care and treatment.
Take home messages
- In Abstract LBA87, the results from the LITESPARK-003 study showed that belzutifan has good anti-cancer effects for patients with advanced kidney cancer when given together with cabozantinib, both as a first anti-cancer medication (group 1) and for patients that had already been treated with immunotherapy (group 2).
- In Abstract LBA88, the results from the LITESPARK-005 study showed that for patients with advanced kidney cancer who had already been treated with immunotherapy or targeted therapy, belzutifan increased the time to when the cancer started growing again compared to everolimus. Also, more patients responded to treatment with belzutifan compared to everolimus. Belzutifan was relatively well tolerated, and no new side effects were reported.
- In Abstract 18810, the results from the LITESPARK-013 study showed that the 120 mg tablet of belzutifan had similar anti-cancer effectiveness to the 200 mg tablet in patients with advanced kidney cancer. Belzutifan was relatively well tolerated, and no new side effects were reported. This study shows that the 120 mg tablet taken every day is the preferred dose of belzutifan for treating advanced kidney cancer.
- In Abstract 18820, the results of the RENOTORCH study showed that treatment with a new immunotherapy infusion called toripalimab (an antibody that blocks the action of PD-1 protein in cancer cells) together with axitinib tablets resulted in a longer time to when the treatment stopped working and the cancer started growing again. More patients with untreated advanced/metastatic kidney cancer responded to treatment with toripalimab plus axitinib compared with sunitinib tablets alone. The results from this study may support the use of toripalimab with axitinib as a first treatment option for advanced kidney cancer. The overall survival information is not available yet.
- In Abstract 1883MO, a phase 1 study with volrustomig, a new immunotherapy that blocks the action of both the PD-1 and CTLA-4 proteins in cancer cells, was presented. This study showed that volrustomig is effective as a first anti-cancer treatment for advanced kidney cancer and for all disease risks (favourable, intermediate, and poor). The side effects were as already reported for immunotherapy treatment.
- In Abstract 1884MO, the TIDE-A study showed that for patients who responded to treatment with the avelumab plus axitinib combination as a first anti-cancer medication, it is safe to stop treatment with axitinib. Having a break from axitinib treatment reduces side effects while keeping the possibility of re-starting axitinib treatment if the cancer starts growing again.
Summaries
Belzutifan for the treatment of advanced kidney cancer
Treatments for people with metastatic kidney cancer have changed over the past several years, resulting in big improvements in patient outcomes and survival. However, unfortunately for most patients their cancer eventually gets worse over time despite treatment.
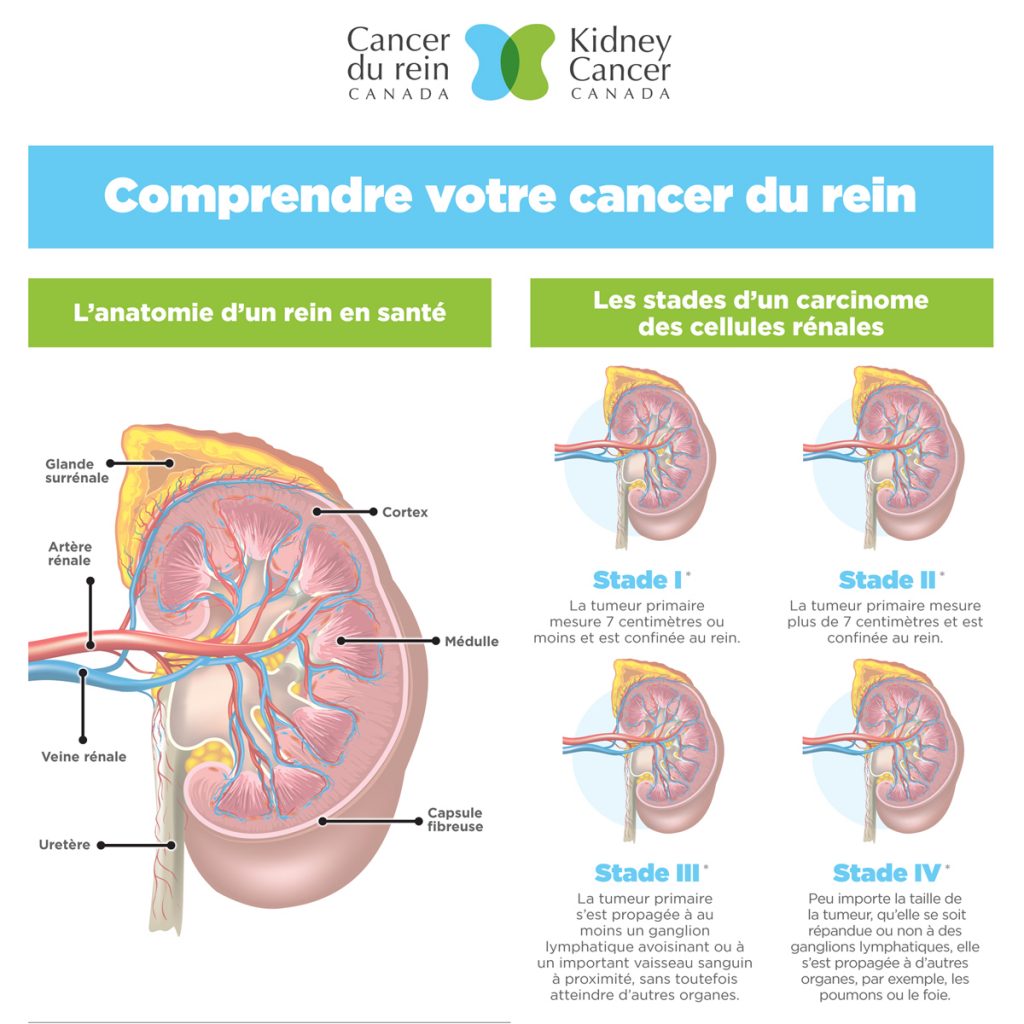
Studies looking at the genes of people with kidney cancer have shown mutations in a gene called the von Hippel-Lindau gene (VHL). This results in high levels of a protein called hypoxia-inducible factor, or HIF-2α in the blood of these patients. This causes changes in the cancer cells that make the tumour grow. A new medicine called belzutifan is a tablet that blocks the action of HIF-2α and, therefore, blocks cancer cell growth.
Belzutifan has been approved in some countries for the treatment of people with VHL disease who develop tumours in the kidney, brain and spinal cord, or pancreas. Belzutifan has also been shown to be effective for the treatment of advanced kidney cancer.
At the ESMO Congress 2023 the results from 3 clinical trials with belzutifan for the treatment of advanced kidney cancer were presented.
Taking belzutifan in combination with cabozantinib shows promise for the treatment of advanced kidney cancer (the LITESPARK-003 study)
Early results from the LITESPARK-003 study showed promising results for belzutifan together with cabozantinib as the first anti-cancer medication (a first-line treatment) for patients with advanced kidney cancer and as a treatment for patients who had already been treated with immunotherapy. Updated results from this study were presented at the ESMO Congress.
LITESPARK-003 is a phase 2 study looking at the safety and effectiveness of belzutifan in combination with cabozantinib, a vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitor (TKI) tablet, in patients with clear cell kidney cancer. The patients were assessed in two groups: Group 1 were patients who had not been treated with anti-cancer medication; group 2 had already been treated with two or less immunotherapies.
There were 50 patients in group 1. After an average follow-up time of 2 years, 6 in 10 patients responded to treatment and their cancer got smaller. One patient had a complete response to treatment and their cancer disappeared. Just over half of the patients had a partial response to treatment. In over a third of patients their cancer was stable. Nearly 6 in 10 patients had a response to treatment that lasted 2 years or more. The average time to when the treatment stopped working and the cancer started growing again (progression-free survival) was just over 2 and a half years for patients in group 1. The average overall survival time could not be measured during the follow-up time.
Nearly half of the patients (46%) in group 1 had serious or life-threatening side effects. There were no deaths in this group of patients.
The study is ongoing for the patients in group 1 (untreated patients) to collect more information about survival.
There were 52 patients in group 2. After an average follow-up time of over 3 years, a third of patients responded to treatment with belzutifan plus cabozantinib and their cancer got smaller. Two patients had a complete response to treatment and their cancer disappeared. More than a quarter of the patients had a partial response to treatment. Six in 10 patients had stable disease. More than half of the patients had a response to treatment that lasted more than 2 years. The average time to when the treatment stopped working and the cancer started growing again (progression-free survival) was just over a year for patients in group 2. Overall survival time was more than 2 years.
Nearly two thirds of patients from group 2 had a serious or life-threatening side effect. Unfortunately, one patient died due to respiratory failure, which was because of the combination treatment.
The results from the LITESPARK-003 study showed that belzutifan has promise as an effective treatment for patients with advanced kidney cancer when given together with cabozantinib, both as a first anti-cancer medication and for patients that have already been treated with immunotherapy.
Belzutifan compared to everolimus in patients with previously treated advanced clear cell kidney cancer (the LITESPARK-005 study)
There were 746 patients with advanced kidney cancer in the phase 3 LITESPARK-005 study. They were randomised to be treated with either belzutifan or everolimus, an mTOR inhibitor tablet. Patients had already been treated with between 1-3 courses of immunotherapy or VEGFR TKI. Patients were followed-up for over 2 years.
The time to when the treatment stopped working and the cancer started growing again (progression-free survival) and the response to treatment were better with belzutifan compared to everolimus. Overall survival time was longer for patients treated with belzutifan, although not statistically significant (21 months compared to 18 months, respectively). 13 patients (3.5%) had a complete response to treatment with belzutifan and their cancer disappeared. There were no complete responses with everolimus. More patients did not have growth of their cancer at 1.5 years with belzutifan compared to everolimus (22.5% compared to 9.0%, respectively).
Nearly three times as many patients stopped treatment because of side effects to everolimus compared to belzutifan. The number of serious and life-threatening side effects were similar for both treatments.
For patients with advanced kidney cancer who had already been treated with immunotherapy or targeted therapy, belzutifan increased the time to when the cancer started growing again compared to everolimus. Also, more patients responded to treatment with belzutifan compared to everolimus. Belzutifan was relatively well tolerated, and no new side effects were reported.
Safety and effectiveness of two doses of belzutifan in patients with advanced kidney cancer (the LITESPARK-013 study)
In a phase 1 study of belzutifan, the maximum dose tolerated by patients for the treatment of kidney cancer was not found. The phase 2 LITESPARK-013 study looked at using a higher dose of belzutifan to see if it improved the effectiveness of the anti-cancer medication while making sure the medicine was tolerated by patients.
There were 154 patients in the study with advanced kidney cancer. Patients had been treated with up to 3 anti-cancer medications, including immunotherapy. Patients were randomly put into two treatment groups: 120 mg tablets of belzutifan every day or 200 mg tablets of belzutifan every day. Patients were followed-up for 20 months.
The response to treatment and progression-free survival were similar for both the 120 mg and 200 mg tablets of belzutifan. The side effects were similar for each tablet. No new side effects were reported.
The 120 mg tablet of belzutifan had similar anti-cancer effectiveness to the 200 mg tablet in patients with advanced kidney cancer. Belzutifan was relatively well tolerated, and no new side effects were reported. This study shows that the 120 mg tablet taken every day is the preferred dose of belzutifan for treating advanced kidney cancer.
Promising new immunotherapies for the treatment of advanced/metastatic kidney cancer
A new first-line treatment, toripalimab, for advanced kidney cancer (the RENOTORCH study)
Advanced/metastatic kidney cancer is often treated with a combination of medicines; either two infusions of immunotherapy (nivolumab and ipilimumab) or immunotherapy (avelumab, pembrolizumab or nivolumab) plus a VEGFR TKI tablet (axitinib, lenvatinib, or cabozantinib).
The phase 3 RENOTORCH study looks at a new immunotherapy infusion (an anti-PD-1 antibody called toripalimab) plus axitinib tablets and compares this combination with sunitinib tablets for the treatment of advanced/metastatic kidney cancer.
There were 421 patients in the study with untreated advanced/metastatic clear cell kidney cancer who had intermediate or poor risk disease. Patients were randomly put into two groups to be treated with either a toripalimab infusion once every 3 weeks plus axitinib tablets or sunitinib tablets alone.
Patients were followed for an average of just over one year. Toripalimab plus axitinib increased the time to when the treatment stopped working and the cancer started growing again (progression-free survival) compared to sunitinib (18 months compared to 9.8 months, respectively). More than half of the patients responded to the combination treatment and their cancer got smaller compared to less than a third for sunitinib. The average overall survival time was not reached for the patients on the combination and was just over 2 years for sunitinib.
Around two thirds of patients reported serious or life-threatening side effects for each treatment, and the number of deaths were similar for each treatment. More patients stopped treatment because of side effects to the combination treatment (14.4% vs 8.1%).
Treatment with the combination of a new immunotherapy called toripalimab plus axitinib resulted in longer progression-free survival and a better response to treatment compared with sunitinib in patients with untreated advanced/metastatic kidney cancer. The results from this study support the use of toripalimab with axitinib as a first treatment for advanced kidney cancer. However, overall survival information is not available yet.
A new immunotherapy, volrustomig, for the first-line treatment of advanced kidney cancer
Blocking the action of programmed cell death protein 1 (PD-1) and cytotoxic T lymphocyte protein 4 (CTLA-4) has been shown to improve survival of patients with advanced kidney cancer. However, CTLA-4 inhibitors, such as ipilimumab, are not well tolerated by some patients. Volrustomig is an immunotherapy that blocks both PD-1 and CTLA-4. This phase 1 study is the first time volrustomig has been given to humans.
Sixty-five patients with advanced kidney cancer were treated with either 750 mg or 500 mg infusions of volrustomig every 3 weeks until their cancer got worse, or they couldn’t tolerate the side effects.
For both doses of volrustomig, nearly half of the patients responded to treatment and their cancer got smaller. More patients had a complete response to treatment and their cancer disappeared at the higher dose (3 patients). The average duration of the response to treatment was just over a year for the higher dose of volrustomig compared to 8.4 months for the lower dose. Time to when the treatment stopped working and the cancer started growing again (progression-free survival) was slightly longer at the higher dose (nearly one year compared to 10 months).
Nearly half of the patients on the higher dose of volrustomig reported a serious or life-threatening immune-related side effect, compared to a quarter on the lower dose. However, nearly half of events did not require steroids and nearly all immune-related side effects that did not affect hormones were treated successfully. There was an increase in the number of T cells in the blood at both doses, and greater activation of T cells with the 750 mg dose of volrustomig compared to the 500 mg dose.
Volrustomig is a new immunotherapy that blocks the action of both the PD-1 and CTLA-4 proteins in cancer cells. This study showed that volrustomig is effective as a first anti-cancer treatment for advanced kidney cancer and for all disease risks (favourable, intermediate, and poor). The side effects were as already reported for immunotherapy treatment. Volrustomig is being looked at as a first treatment option for advanced kidney cancer in combination with lenvatinib.
Combination treatments for advanced/metastatic kidney cancer
In many countries, combinations of VEGFR TKI anti-cancer mediations plus immunotherapies are the standard of care as the first anti-cancer treatments for patients with advanced/metastatic kidney cancer due to increased response to treatment, longer progression-free survival and longer overall survival times compared to VEGFR TKI alone. It is known that most of the side effects from these combinations of anti-cancer medications are due to the VEGFR TKI.
Combinations of treatments continue to be of interest. But there remains the question of which combination of treatments is best for an individual patient with advanced/metastatic kidney cancer?
Does stopping VEGFR TKI treatment and continuing with immunotherapy treatment influence the survival of patients with metastatic kidney cancer being treated with an immunotherapy (avelumab) plus VEGFR TKI (axitinib) combination? (The TIDE-A study)
In this phase 2 study, metastatic kidney cancer patients were treated with a combination of avelumab infusions every 2 weeks plus axitinib tablets daily for 36 weeks. At 36 weeks, the patients who had a response to treatment and their cancer got smaller stopped axitinib and continued with avelumab until their cancer started growing again (disease progression) or they couldn’t tolerate the side effects. If their cancer got worse, they re-started axitinib for 24 weeks. If they had another response to treatment, axitinib was stopped again and treatment with avelumab was continued. Patients with stable disease at 36 weeks continued the combination until their cancer started growing again or they couldn’t tolerate the side effects.
75 patients were assessed for the effectiveness of this treatment schedule. Nearly 4 in 10 patients stopped treatment with axitinib at 36 weeks. Three quarters of patients responded to treatment and their cancer got smaller and nearly one fifth of patients had stable disease. The time to when the treatment stopped working and the cancer started growing again was nearly 2 years, and for 7 in 10 patients their cancer did not grow for at least 18 months. The average length of the first axitinib break was 16 weeks. Of the 29 patients who stopped treatment with axitinib, 9 are still ongoing. For the other 20 patients, their cancer got worse. Of these, 19 re-started treatment with axitinib.
More than 9 in 10 patients had at least one side effect to treatment, and 4 in 10 had a serious or life-threatening side effect. There were no treatment-related deaths. A third of all patients reported side effects to axitinib, and 1 in 10 of all patients reported serious or life-threatening side effects to axitinib.
The TIDE-A study shows that for patients who responded to treatment with the avelumab plus axitinib combination as a first anti-cancer medication, it is safe to stop treatment with axitinib. Having a break from axitinib treatment reduces side effects while keeping the possibility of benefiting from axitinib treatment if it is re-started.
Acknowledgements:
Editor: Dr Ravindran Kanesvaran (SG)
Medical Reviewer: Dr Eric Jonasch (US) and Professor Axel Bex (NL/UK)
Medical Writer: Dr Sharon Deveson Kell (UK)