Highlights from the ESMO Congress 2022
Source: International Kidney Cancer Coalition (IKCC)
The European Society for Medical Oncology (ESMO) congress was held in person (for the 1st time in 2 years) and virtually from 9-13 September 2022. The presentations are available to view on the ESMO website if you have previously logged in to the site. The International Kidney Cancer Coalition (IKCC) attended the scientific programme to keep abreast of the latest advances in the care and treatment of people with kidney cancer.
Please note: The following summary was prepared by patient advocates for the benefit of patient organisations around the world who focus on kidney cancer. While this summary has been medically reviewed, the information contained herein is based upon public data shared at this meeting and is not intended to be exhaustive or act as medical advice. Patients should speak to their doctor about their own care and treatment.
Do adjuvant treatments with immunotherapies work for patients with a high risk of their cancer coming back?
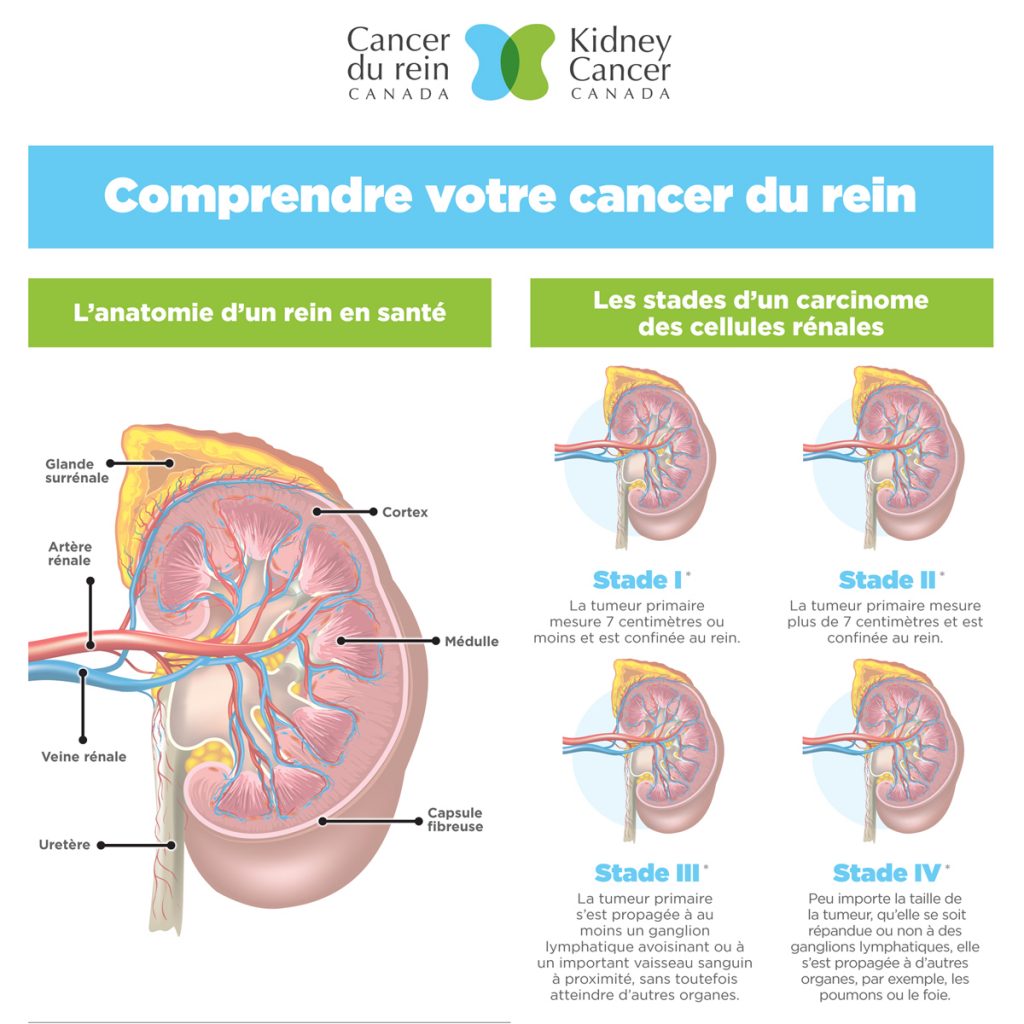
Surgery (nephrectomy) is the standard of care for localized kidney cancer; however, the cancer can come back (recurrence) after nephrectomy. Adjuvant therapy is medication that is given after surgery to try to prevent the cancer from coming back.
In the past, vascular endothelial growth factor (VEGF) tyrosine kinase inhibitor (TKI) tablets and cytokines have been tested as adjuvant therapies for kidney cancer. The benefit of these treatments for patients has been inconsistent, and they have significant side effects. This limits their use and for many patients their cancer comes back months or sometimes years later.
Does adjuvant nivolumab plus ipilimumab work at reducing the return of localised kidney cancer at high risk of coming back after surgery?
abstract LBA4In a recent phase 3 clinical trial (CheckMate 914) the combination of nivolumab plus ipilimumab was assessed as an adjuvant treatment for people with localised kidney cancer. In total, 816 people participated in this study. All these people had recently undergone full or partial removal of their kidney and were at moderate or high risk of their cancer returning.
Patients were randomly chosen to receive either the combination of nivolumab plus ipilimumab, or placebo (an infusion without any active medicines). The results showed that treatment with nivolumab plus ipilimumab was no better than placebo at preventing the cancer from coming back (also known as disease-free survival) and did not improve overall survival compared to placebo. Patients who received nivolumab plus ipilimumab had quite a few more side effects. Also, it is an expensive treatment. The safety of nivolumab plus ipilimumab was like that reported in other clinical trials.
The study is continuing with nivolumab alone compared to placebo.
Does atezolizumab work as an adjuvant therapy in patients with localised kidney cancer at increased risk of coming back after surgery?
abstract LBA66IMmotion010 is a phase 3 randomised study that compares atezolizumab with placebo. The study is double-blind, meaning that the doctor and the patient do not know which treatment the patient is given. The effectiveness of atezolizumab was assessed as an adjuvant therapy in patients with localised kidney cancer with an increased risk of recurrence after surgery.
778 patients were treated for one year with either atezolizumab infusions or placebo infusions every 3 weeks. The average follow-up time was just over 3 and a half years. Average disease-free survival was nearly 5 years (57.2 months) for patients on atezolizumab and just over 4 years (49.5 months) for patients on placebo, and this difference was not considered to be “statistically significant”, meaning the study failed to show a delay in cancer recurrence in the atezolizumab-treated group of participants.
Serious or life-threatening side effects occurred in 27% of patients on atezolizumab and 21% of patients on placebo. There were less than 1% of deaths in each group, none related to treatment.
In conclusion, adjuvant atezolizumab did not significantly delay the return of the cancer when compared to placebo after surgery for localised kidney cancer.
Can the use of nivolumab before and after surgery prevent recurrence of kidney cancer in high-risk patients?
abstract LBA67In this phase 3, randomised study the immune system was stimulated with nivolumab before surgery (neoadjuvant therapy) followed by adjuvant nivolumab in patients with high-risk localised kidney cancer. This was compared to surgery alone.
There were 819 patients in the study who were allocated to two groups. In the treatment group, patients were given one dose of nivolumab 4 weeks before surgery followed by 9 doses every four weeks after surgery. The control group had surgery followed by observation alone.
Recurrence-free survival was similar in both groups of patients and the study was stopped early because of lack of effectiveness. Average recurrence-free survival and overall survival times were not reached but were similar for both groups of patients. Serious or life-threatening side effects were reported by 20% of patients treated with nivolumab, compared with 6% in the control group.
This study showed that nivolumab given before and after surgery did not improve recurrence-free survival in kidney cancer patients who are at high risk of their cancer returning.
Looking at new combinations of treatments for kidney cancer
Is bempegaldesleukin plus nivolumab better than a VEGF TKI tablet for previously untreated patients with advanced kidney cancer?
abstract LBA68Despite advances in first-line treatments for advanced kidney cancer over the past few years, new treatments are on the horizon. This study looked at a new medicine called bempegaldesleukin in combination with nivolumab for the treatment of patients with advanced kidney cancer. Patients in all International Metastatic Renal Carcinoma Database Consortium (IMDC) risk groups (favourable, intermediate, and poor) were accepted in this study, as were patients with some impairment of their daily living (Karnofsky score of 70). Bempegaldesleukin is a modified form of a cytokine called interleukin 2. The modifications alter the way interleukin 2 binds to cells, favouring one place where the interleukin-2 binds to the cell surface (a receptor), over another.
PIVOT-09 is a phase 3, randomised trial of bempegaldesleukin in combination with nivolumab compared to VEGF TKI tablets, also known as targeted therapies for previously untreated kidney cancer patients with advanced or metastatic disease.
623 patients were enrolled in the study and allocated to two equal groups to be treated with a bempegaldesleukin plus nivolumab infusion every 3 weeks or a VEGF TKI tablet (sunitinib or cabozantinib).
After an average follow-up time of 15.5 months, 23% of patients in the bempegaldesleukin plus nivolumab group compared to 30.6% in the TKI group responded to treatment and their cancer got smaller. Average overall survival time was 29 months for the patients in the combination group and wasn’t reached in the TKI group, showing that the experimental treatment was not superior to standard TKI therapy.
The most common side effects in the bempegaldesleukin plus nivolumab group were a high temperature, itchy skin, feeling sick (nausea), higher than normal levels of white blood cells, an overactive thyroid gland, rash, and joint pain. More than a quarter of patients had serious or life-threatening side effects, and 3 patients died.
In this study with previously untreated patients with advanced or metastatic kidney cancer, bempegaldesleukin plus nivolumab did not improve survival compared to TKI treatment.
The effectiveness of a triple combination of cabozantinib, nivolumab and ipilimumab for previously untreated patients with advanced kidney cancer with high-risk disease
abstract LBA8Cabozantinib, a type of VEGF TKI tablet (or targeted therapy) acts by blocking several types of receptors on the cell surface, including MET, VEGF, and TAM kinases. It also may enhance the action of immunotherapy drugs. The combinations of cabozantinib plus nivolumab and ipilimumab plus nivolumab are both used in several countries as a first treatment for people with advanced kidney cancer, especially cancer that is of moderate or high risk, as defined by some straightforward factors, including low red blood cell count, and time from diagnosis to needing treatment for the cancer.
COSMIC-313 is the first study to combine cabozantinib with nivolumab and ipilimumab, two intravenous immune-stimulating therapies, and compare it to ipilimumab plus nivolumab for the treatment of people with moderate- or high-risk advanced kidney cancer.
855 patients were assessed in this phase 3 study. Patients were randomly allocated to receive either nivolumab and ipilimumab plus cabozantinib or nivolumab and ipilimumab plus placebo. The study is double-blind, meaning both the doctor and the patient do not know which treatment they are on. All patients had clear cell kidney cancer that was of moderate or high risk.
Preliminary results from the clinical trial have been released. The results showed that adding cabozantinib to nivolumab plus ipilimumab increased the time to when the treatment stopped working and the cancer started growing again (progression-free survival). Average progression-free survival was not reached for the triple combination, but for the ipilimumab plus nivolumab combination it was just over 11 months.
Whether the three-drug combination increased overall survival times for the triple combination compared to nivolumab plus ipilimumab was not reported, and the trial is ongoing to collect this information. The cancer got smaller in 43% of the patients who were on the triple combination, compared to 36% on ipilimumab plus nivolumab. Only three percent of patients in either arm had complete disappearance of their disease, a disappointingly low number.
Serious or life-threatening side effects were reported by 73% of patients taking the triple combination and 41% on ipilimumab plus nivolumab, with liver inflammation occurring in more patients who received the three-drug combination. There were 3 deaths (1%) in each treatment group that were related to treatment. 12% and 5% of patients stopped treatment in the triple combination group and ipilimumab plus nivolumab treatment group, respectively.
In summary, the triple combination of cabozantinib, nivolumab and ipilimumab prolonged the time to when the treatment stopped working and the cancer started growing again compared to ipilimumab plus nivolumab in patients with previously untreated advanced kidney cancer with moderate- or high-risk disease. However, as of now we do not know if the triple combination improves survival. We also see a low percentage of patients with complete disappearance of their disease, and a lot of toxicity. We need more time and information to determine whether this three-drug combination should be considered as a preferred treatment regimen.
Looking at alternative treatment schedules for TKIs and immunotherapy
Can treatment with nivolumab and nivolumab plus ipilimumab in metastatic kidney cancer be personalised?
abstract 1450MOIf kidney cancer spreads (becomes metastatic), medicines can help control the cancer to prolong life and decrease the symptoms caused by the cancer. For the past decade, the main treatments have been TKI tablets that block the blood supply to the tumour to stop the growth of the cancer. In the last few years, research has shown that immunotherapies to stimulate the patient’s own immune system against the cancer have been successful in some people.
Two of the first immunotherapy medicines to be approved were nivolumab plus ipilimumab. This combination is given every 3 weeks for 3 months (four treatments) as an infusion followed by a nivolumab infusion for up to 2 years if there is response.
The TITAN-RCC study wanted to see if a more personalised approach will improve the outcomes and experience of people taking immunotherapy. Patients started treatment with nivolumab alone and then used nivolumab plus ipilimumab only if needed as a boost to control the cancer.
207 patients with moderate or high-risk metastatic kidney cancer were enrolled in the study. About half of these people had never taken a treatment before; the other half had been treated with a TKI tablet. The patients started with nivolumab infusions every 2 weeks. After 16 weeks, those patients who had stable disease or whose cancer had got worse (had not responded to treatment) were treated with the ipilimumab plus nivolumab combination (2-4 doses). Patients who responded to nivolumab alone, continued with nivolumab, but could be given the combination if their cancer got worse.
Of the people who had not previously been treated, 28% responded to nivolumab alone and their cancer got smaller. For people who had been treated with a TKI before the study, 18% responded to nivolumab alone.
Throughout the study, 44% of previously untreated and 53% of previously treated patients were given ipilimumab boosts because their cancer got worse. For all patients, after an average follow-up of nearly 16 months, the cancer responded by getting smaller in 36% of the patients who had not previously been treated, and 32% of the patients who had been treated with a TKI tablet before the study. For previously untreated patients, the average time to when the treatment stopped working and the cancer started growing again was 6.3 months and 3.7 months for previously treated patients. Overall survival time was 32 months and 25.9 months, respectively.
This study shows that adding ipilimumab in a delayed fashion after nivolumab treatment modestly boosts disease shrinkage and time to disease progression compared to nivolumab alone. Responses to treatment with the combination were also seen after the cancer got worse during the nivolumab maintenance treatment. However, the overall effectiveness of this personalised approach seems to be inferior to upfront ipilimumab plus nivolumab combination treatment, and really isn’t a recommended approach.
Update of the lenvatinib plus pembrolizumab versus sunitinib study in patients with advanced kidney cancer
abstract 1449MOResults from the phase 3 CLEAR study showed that lenvatinib (a VEGF TKI tablet) used together with pembrolizumab (an immunotherapy infusion) resulted in better survival and cancer shrinkage compared to sunitinib when used for patients with advanced kidney cancer who had not been treated before. Updated information from patients who completed 2 years of pembrolizumab plus lenvatinib treatment and continued lenvatinib treatment alone are presented.
There were 1069 patients in this study, who were put into 3 groups: one group were treated with lenvatinib plus pembrolizumab, another group with lenvatinib plus everolimus, and the third group with sunitinib. Patients were followed up for nearly 3 years.
For patients treated with lenvatinib and pembrolizumab, the time to when the treatment stopped working and the cancer started growing again (progression-free survival) was nearly 2 years, compared to 9.2 months for sunitinib. The duration of response to treatment was longer for the patients taking lenvatinib plus pembrolizumab (26 months) compared to sunitinib (14.7 months).
Of the patients who completed 2 years of pembrolizumab plus lenvatinib treatment, most had moderate or high-risk kidney cancer. The overall survival time for the patients who completed 2 years of combination treatment was 3 years. Of these patients, 68% had treatment-related side effects and were more likely to have a reduction in their dose of treatment as (around two thirds of patients) than patients in the sunitinib group (around half of patients). However, the side effects for each treatment were not unexpected and were manageable.
71% of patients responded to treatment with lenvatinib plus pembrolizumab and their cancer got smaller compared with 36.1% for sunitinib. 17.2% of patients on the combination had a complete disappearance of their tumours in comparison with 4.2% for those on sunitinib. The median duration of response was 26 months with lenvatinib plus pembrolizumab compared with 14.7 months with sunitinib.
The lenvatinib plus pembrolizumab combination continues to show better tumour shrinkage, delay in cancer growth and overall survival compared to sunitinib. A large proportion of patients treated with the combination completed 2 years of treatment and continued with lenvatinib treatment with ongoing clinical benefit. The results further support lenvatinib plus pembrolizumab as a potent combination therapy for previously untreated advanced kidney cancer patients. However, the combination of lenvatinib and pembrolizumab also shows several side effects, and patients and the healthcare team need to work together closely to ensure that appropriate treatment breaks and dose reductions occur to maintain good quality of life.
Potential biomarkers for kidney cancer treatments
Up to 1/3 of kidney cancer cases are diagnosed when the cancer has already spread to other tissues and organs (stage 4). Patients with stage 4 or metastatic kidney cancer have poor outcomes, and less than half of them will survive for 5 years. Doctors need a way to assess the effectiveness of medicines for metastatic kidney cancer and to monitor the progress of the disease.
Biomarkers are naturally occurring substances in the body that can be used to assess the progress of a disease or a body process. Biomarkers can be liquid biomarkers that are found in the blood, genetic biomarkers, or tissue biomarkers found in tumour tissue. Biomarkers can be used to assess the response of disease to treatment. They can also be used to monitor the status of the disease over time and predict recurrence of progression.
Tumour biomarkers to predict the effectiveness of nivolumab with or without ipilimumab in previously untreated patients with metastatic kidney cancer
abstract 1451MOThe phase 2 BIONIKK trial recently found genetic biomarkers that are potentially linked to better response to treatment with immunotherapy infusions and VEGF TKI tablets in previously untreated patients with metastatic kidney cancer. This study further identified biomarkers for the effectiveness of nivolumab with or without ipilimumab using immune biomarkers from tumour tissue samples.
The researchers looked at samples of tumour tissue and identified the main immune cells, such as T cells, B cells, tertiary lymphoid structures, and biomarkers of immune activity called Ki67+PD1+ cells.
160 patients with metastatic kidney cancer had tumour samples taken. In patients treated with nivolumab, more than two tertiary lymphoid structures were associated with a better response to treatment, longer time to when the drug stopped working and the cancer starts growing again, and less early progression of the cancer.
In patients treated with nivolumab plus ipilimumab, more than two tertiary lymphoid structures again indicated a better response to treatment. More Ki67+PD1+ cells were associated with a longer time to when the drug stopped working and the cancer started growing again and less early progression of the cancer.
Combining these two biomarkers (tertiary lymphoid structures and Ki67+PD1+ cells) researchers were able to identify patients with both high response rates (80% versus 43%) and less early progression of their cancer (5% vs 36%).
This randomised biomarker study showed that the number of tertiary lymphoid structures (which is similar in the lymph nodes of a person without kidney cancer) and ki67+PD1+ cells are likely to predict the effectiveness of nivolumab with or without ipilimumab in previously untreated metastatic kidney cancer patients. A combination of these biomarkers helps researchers identify patients with improved outcomes with nivolumab and ipilimumab.
A shift in gut bacteria during standard therapies for metastatic kidney cancer
abstract 1452MOThe bacteria in the gut play a vital role in developing immunity to disease and may be able to control the immune response caused by immunotherapy in people with cancer. This study looked at the kidney cancer risk (favourable, intermediate, or poor) compared to the bacteria in the gut after treatment with TKI tablets and changes in gut bacteria during immunotherapy infusions and TKI treatment.
Stool samples were collected from people with metastatic kidney cancer who had started treatment with immunotherapy or a TKI as their first, second or later treatment. Stool samples were collected before and during treatment (within 1, 3, 6 and 12 months of the start of treatment).
There were 127 patients in the study. In 48% of patients on TKIs their cancer got smaller, and they responded to treatment. However, more than half of these patients had diarrhoea. For the immunotherapy patients, 31% of patients responded to treatment. Overall, the researchers noted differences in the types of bacteria in the gut between the treatment groups.
In this study, the researchers concluded that in contrast to immunotherapy treatment, TKI treatment resulted in more harmful gut bacteria, despite treatment success. TKIs increased bacteria related to the development of cancer, weight loss, loss of muscle mass, and inflammation. This was possibly due to gut toxicity. These data may influence decision-making for the first treatment and subsequent sequencing of treatments for metastatic kidney cancer.
Update on treatment for von Hippel-Lindau disease
Belzutifan for von Hippel-Lindau (VHL) tumours: 3 years of follow-up
abstract LBA69Kidney cancers frequently have mutations in the von Hippel-Lindau (VHL) gene, resulting in high levels of a protein called hypoxia-inducible factor, or HIF-2α. This results in several changes in the cancer cells and their surrounding environment that favour tumour growth. The novel hypoxia-inducible factor 2α (HIF-2α) inhibitor, belzutifan, blocks the action of HIF-2α.
Belzutifan is the first oral HIF-2α inhibitor approved for patients with VHL disease who require treatment for associated kidney cancers, CNS hemangioblastomas, or pancreatic neuroendocrine tumours (pNET) that do not need immediate surgery. This study presents more than 3 years of follow-up from the phase 2 LITESPARK-004 study.
People with the mutated VHL gene and one or more kidney cancer tumours that had not spread outside the kidney were included in the study. None of the tumours needed immediate surgery and none of the patients had been previously treated.
61 patients were enrolled in the study. After more than 3 years, 38 patients (62%) remain on treatment. The primary reasons for stopping treatment were the patient’s decision (18%) and disease progression (10%). Of the 61 patients with kidney tumours, 63% responded to treatment and their tumours got smaller. Average time to tumour shrinkage was just over 11 months. The other non-kidney cancer related tumours also continued to show very good response to treatment.
Serious side effects were reported by 18% of patients. Low red blood cells (anaemia) were the most common side effect (11%). There were no life-threatening side effects or deaths, or no new side effects reported in the additional follow-up.
After an average follow-up of more than 3 years, belzutifan continues to be an effective treatment and has long-lasting responses in patients with VHL disease. Belzutifan was well tolerated, and the side effects were manageable.
Poster presentations
- 1474P: The main objective of this study was to look at the role of a biomarker called the PD-L1 receptor to predict the outcome of patients with metastatic kidney cancer who had only been treated with VEGF TKI tablets. A total of 242 patients had their tumour tissue assessed for the PD-L1 receptor. Average overall survival time in patients with high levels of the PD-L1 receptor was 14.5 months, and 9.7 months with low levels of the receptor. This was more obvious in patients with favourable risk kidney cancer, who had average overall survival times of more than 3 years. This study suggests that the PD-L1 receptor in tumour tissue can be used to predict survival in patients with metastatic kidney cancer.
- 1464P: This observational study looked at the effect of poor kidney function on the use of immunotherapies for the treatment of metastatic kidney cancer in the real world. Of 1059 kidney cancer patients with poor kidney function, more than three quarters were treated with a combination of ipilimumab plus nivolumab, while the remainder were treated with a VEGF TKI tablet as a first treatment. The study showed that renal function does not reduce the effectiveness of immunotherapy combinations given as a first treatment for metastatic kidney cancer. Doctors should not restrict access to these treatments based on renal function, which is important for patients who have had a nephrectomy.
- 1457P: Patients with brain metastases from the spread of kidney cancer often have poor outcomes. This study looked at real world data from the UK on patients with kidney cancer brain metastases. The number of people with brain metastases and their survival were analysed. 1173 patients with kidney cancer were identified. Of these 154 patients had brain metastases (13.1%), 80% of which did not have any symptoms. This study showed that there were more people with brain metastases than first thought. Also, overall survival time for patients who were treated with immunotherapy before the diagnosis of brain metastases was longer than those who were treated after diagnosis of brain metastases or who were not treated with immunotherapy. The researchers suggest the use of immunotherapy as a first treatment after surgery and routine brain scans to improve survival. It might be important for poor risk cases.
- 1458P: This study looked at the association of health-related quality of life and clinical outcomes in patients with metastatic kidney cancer. The research was based on data from the CheckMate 9ER study. Patients were randomised to nivolumab plus cabozantinib or sunitinib. There was a positive association between health-related quality of life and overall survival time, time to when the medicine stopped working and the cancer started growing again, and response rate (how much the cancer got smaller) in this study. Patients continued to report improved quality of life with the combination compared to sunitinib, regardless of side effects. Patient-reported outcomes may be useful for describing the patient’s experience during a clinical trial and predicting clinical outcomes during routine clinical practice. This is an example of the relevance of patient-centred care.
- 1453P: This poster updated the results from an ongoing small phase 2 study, where the safety and efficacy of belzutifan in combination with cabozantinib was assessed in kidney cancer patients who had been previously treated with immunotherapy or who were untreated. There were 52 patients in the study, who were followed for an average of just over 2 years. Belzutifan plus cabozantinib continued to show promising anti-cancer activity in patients with metastatic kidney cancer that had been previously treated. Belzutifan plus cabozantinib is a safe combination and there were no life-threatening side effects and only one treatment-related death. However, these data are not very different from an older study that tested belzutifan alone in a similar patient population (Choueiri and Jonasch, Lancet Oncology 2021). It is important to consider the trade-off between potential increased effectiveness of combination treatment versus both the physical and financial toxicity associated with taking more drugs at the same time.
- 1461P: This study looked at the first treatment given to patients with a subtype of kidney cancer called MiT family translocation renal cell carcinoma. This is an aggressive cancer with very few treatment options. 56 patients were included in the study and treated first with an immunotherapy. They were followed-up for just over 2 years. Average overall survival time was 13.5 months for patients on immunotherapy, compared to 3 years for patients who did not receive immunotherapy. This study showed that some translocation patients do not benefit from immunotherapy as a first treatment. The study highlights the poor outlook for patients with this subtype of kidney cancer. These findings also help to personalise treatment for patients with rare subtypes if kidney cancer.
- 1471P: This study looked for a biomarker called kidney injury molecule-1 (KIM-1) in the blood to see if KIM-1 could help decide the risk of surgery in patients with a kidney mass. The presence of KIM-1 in the blood before surgery helped to determine between benign and malignant kidney masses. In patients with kidney cancer, high KIM-1 levels before surgery were associated with worse survival. Blood levels of KIM-1 may be useful for the diagnosis of kidney cancer, either alone or in combination with other biomarkers. Further work is ongoing and external checking of these results are needed to confirm these findings.
ACKNOWLEDGEMENTS:
Editor:
Dr Stenio Zequi (BR)
Medical Reviewers:
Dr Rachel Giles (NL)
Dr Michael Jewett (CA)
Dr Eric Jonasch (USA)
Medical Writer:
Dr Sharon Deveson Kell (UK)